The healthcare industry is going through a seismic shift. The old fee-for-service (FFS) model, which rewarded providers for the number of services delivered, is giving way to value-based care. This new approach prioritizes patient outcomes and cost efficiency over sheer volume. For healthcare providers, this transformation means rethinking their strategies, especially when it comes to RCM for Value-Based Care.
What Is Value-Based Care?
At its heart, value-based care rewards healthcare providers for delivering better patient outcomes. It’s about quality over quantity, focusing on making patients healthier, improving their experience, and reducing overall costs.
But transitioning to value-based care isn’t simple. It involves overhauling systems and processes that were built for the FFS model. By 2025, it’s estimated that most U.S. healthcare payments will be tied to value-based care models, pushing organizations to adapt quickly.
How Value-Based Care Impacts RCM
Revenue cycle management (RCM) is the backbone of healthcare operations, and under value-based care, it must evolve to meet new demands. Here’s how RCM for Value-Based Care is adapting:
1. Seamless Data Integration
Value-based care requires clinical and financial systems to work together seamlessly. Interoperability ensures providers have real-time patient data for better decision-making.
- Example: Imagine a healthcare call center verifying a patient’s insurance details before their appointment, ensuring accurate claims and fewer billing errors.
Stat: 78% of healthcare executives consider improving interoperability a top priority for value-based care.
2. Managing Complex Payment Models
Value-based care introduces new payment methods, such as bundled payments and shared savings. These models demand robust systems to handle complex arrangements and ensure accurate reporting.
- Example: A patient undergoes a hip replacement. The call center confirms their bundled payment coverage, avoiding unexpected bills and ensuring financial clarity.
Stat: Bundled payments reduce costs by 5.6% per episode of care without compromising quality.
3. Proactive Denial Management
With value-based care, claims undergo greater scrutiny. Proactive denial management—like accurate coding and preauthorization—helps reduce rejections.
- Example: Call centers assist in gathering necessary documentation and following up on denied claims, speeding up the resolution process.
Stat: 65% of claim denials are preventable with proper front-end processes.
4. Focusing on the Patient’s Financial Experience
Transparent billing is critical in value-based care. Patients want clear communication about their financial responsibilities.
- Example: Call centers provide financial counseling, breaking down bills and offering payment plans, increasing patient satisfaction and timely payments.
Stat: 87% of patients want more clarity on their bills; 61% would switch providers over billing issues.
5. Supporting Population Health Management
Value-based care isn’t just about treating illnesses; it’s about prevention and chronic disease management. Aligning RCM for Value-Based Care with population health initiatives ensures better outcomes and financial rewards.
- Example: A call center schedules reminders for diabetic patients, ensuring regular checkups and avoiding costly complications.
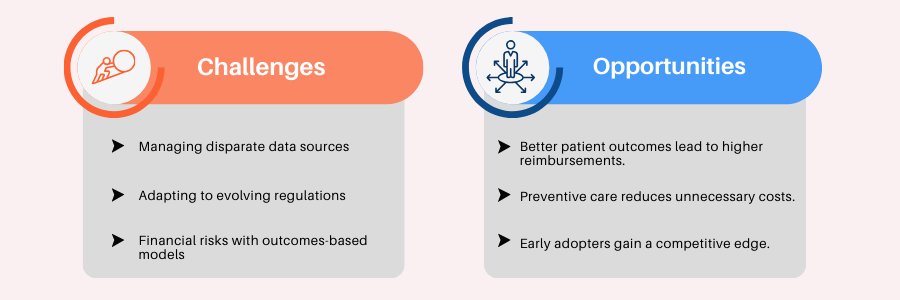
Challenges and Opportunities
Why Call Centers Are Essential for Value-Based RCM
Call centers aren’t just about answering phones—they’re the unsung heroes in the transition to value-based care. Here’s how they help:
1. Educating Patients
Clear communication helps patients understand their care plans and financial responsibilities, leading to fewer disputes and smoother claims.
Example: A patient learns about their deductible and treatment costs upfront, avoiding surprises later.
2. Real-Time Verification
Ensuring insurance eligibility and coverage reduces claim denials.
Example: Call centers verify coverage before surgery, ensuring the procedure aligns with the patient’s plan.
3. Denial Management
Quick follow-ups and appeals minimize revenue losses.
Example: A rejected claim is resolved within days, thanks to prompt call center action.
4. Enhancing Care Coordination
From appointment reminders to chronic care follow-ups, call centers keep patients engaged and on track.
Example: Follow-ups for heart failure patients reduce hospital readmissions by 20%.
Why Fusion CX Is the Right Partner
Fusion CX is at the forefront of RCM for Value-Based Care transformation. Here’s what makes us stand out:
- Expertise: We specialize in RCM for Value-Based Care, understanding its unique challenges and opportunities.
- Advanced Technology: Our AI-driven tools streamline claims processing and provide actionable insights.
- Global Reach: With operations in 15 countries, we offer scalable solutions for healthcare organizations of all sizes.
- Patient-Centric Focus: Clear communication and patient education are at the heart of what we do, ensuring better engagement and compliance.
The move to value-based care is reshaping healthcare delivery and financial management. Call centers play a pivotal role in this transformation, ensuring smoother communication, better patient outcomes, and optimized revenue processes. By partnering with Fusion CX, healthcare providers can navigate this transition confidently, achieving sustainable growth while delivering exceptional care.